Minas Constantinides, Andres Bustillo, and Anil Shah
Rhinoplasty is among the most challenging of facial plastic surgical procedures. Not only is the nose the central aesthetic feature of the face, but also, if it is misshapen, a functional problem may compound the cosmetic distortion. Potential difficulties the surgeon might encounter in primary rhinoplasty are made only more challenging when the patient has already had one attempt at surgery.
Revision rhinoplasty is not simply a second surgery in the same anatomic location. At best, the patient wants a little better result than the one he or she was left with after one surgery. At worst, the patient is devastated by a crippling functional problem coupled with a deformity lying in the middle of the face. The high expectations the revision rhinoplasty patient places on the surgeon make accurate preoperative diagnosis imperative. The surgeon must have the skill to analyze a deformity, decide how to repair it, and have several alternatives available if the diagnosis is inaccurate or the technique of repair is suboptimal. Anatomic variations, already a challenge to the primary rhinoplasty surgeon, become hurdles of uncertainty the revision surgeon must overcome through accurate diagnosis and sound repair.
Although the techniques for analyzing an unoperated and a previously operated nose are the same, the underlying structure and anatomy may be vastly different. Proper correlation between analysis and aberrant anatomy will lead to more successful outcomes in revision rhinoplasty.
History
Patients seeking revision rhinoplasty tend to be highly selective in their choice of surgeon. Their revision surgery represents a significant financial, emotional, and time- consuming investment, and patients are naturally more apprehensive about their subsequent procedure. The surgeon must restore the patient’s confidence while mitigating realistic outcomes.
Each patient consulting for revision rhinoplasty has vastly different expectations; the surgeon should advise the patient about how pragmatic these expectations are. An open consultation will help the patient to understand the difficulty and degree of improvement in correcting specific nasal deformities. For example, a patient with an overly narrowed nostril sill caused by overly aggressive Weir excisions should be advised of the challenge that revision surgery represents.
During the interview, it is important to seek out not only aesthetic change but also functional issues. Often, patients with longstanding nasal obstruction do not realize their degree of nasal airflow impairment. This is especially true in patients with uncorrected septal deviations from previous surgeons and narrow internal valves.
Patients ideally should obtain before and after photographs for each nasal operation and the previous surgeon’s operative notes. Unfortunately, a previous rhinoplasty surgeon’s operative history may harbor gross inaccuracies and should only be used as a rough guide. Photographs may demonstrate a temporal relationship between the complication and when it occurred. An illustration of this is the dynamics of middle vault narrowing, which occurs gradually over a period of years rather than months. The patient’s pictorial record may demonstrate subsequent narrowing and coinciding nasal obstruction.
Physical Examination
Correlation of the physical exam with controlled quality photographic stills of the patient will provide a better understanding of the patient’s residual nasal deformity. Each of these necessary diagnostic arms provides information that complements the other.
The thickness and character of the skin-soft tissue envelope (S-STE) should be determined. Patients with previous surgery may have extensive thinning of the skin, damage caused by extrusion of alloplastic implants, or significant scarring with thickening. Palpation of the S-STE will reveal the extent of damage and mobility of the skin, which may temper expectations of both patient and surgeon. For instance, in a patient seeking dorsal augmentation and added length to his nose, a severely scarred and contracted envelope will limit the amount of surgical improvement possible.
The bony pyramid is examined and palpated for asymmetries, irregularities, and width. The nasal dorsum should follow a gentle curving line from the medial brow to the tip. Persistent dorsal humps should be palpated to help identify their constitution. When the middle vault is examined, it is important to note any asymmetries, the width, deviations, and saddling. Collapse of the upper lateral cartilages (ULC) also should be noted. It is imperative to examine the dorsal septum in the middle vault area. Deviations in the middle vault can be caused by upper lateral cartilage depressions, dorsal septal deviations, or both.
The tip’s rotation, projection, and its relation to the dorsum are then evaluated. Domal asymmetries, fullness, depressions, and the overall shape of the nasal tip should be noted. Palpation of the cartilaginous framework is essential to diagnose the deformity. Tip strength should be determined to successfully plan the reconstruction of the medial and lateral tip components and determine the residual strength of the nasal base. The nasal-labial angle is examined next. Its contributions from the nasal spine and posterior septal angle should be palpated to distinguish soft tissue from cartilaginous excess. Although frequently overlooked, the position of the nasal tip also can contribute to nasal obstruction. Ptotic tips should be manually elevated to determine whether any improvement to the obstruction occurs.
The functional examination begins by watching the patient breathe. Does the patient breathe primarily through the mouth or the nose? When breathing through the nose, is there dynamic collapse with normal inspiration? When breathing more forcefully, which side collapses first or most severely?
The intranasal examination concentrates on each nasal functional subsection independently. The external nasal valves, septum, internal nasal valves, inferior turbinates, middle meatuses, and nasopharynx are examined serially. Inspection of the nasal septum for any residual deviations and contributions, if any, to dorsal deviations is performed. Any crusting must be removed to reveal the condition of the mucoperichondrium and possibility of occult nasal perforation. The presence of perforations should be noted and explained to the patient. Although perforations may be complications of previous surgeries, the patient’s social history should be reviewed to determine drug consumption. The septum may be palpated with a cotton tip applicator to help determine whether cartilage is present. In addition, both auricles should be palpated to determine the amount and character of residual cartilage of the concha cymba and cavum. Turbinate hypertrophy should be noted, and the nasal mucosa and vestibule should be examined for scaring or webbing. Webbing is a common source of postoperative nasal obstruction, often caused by scarring or failure to properly close endonasal incisions.
Next, a careful analysis is performed of the external and internal nasal l incisiovalves. No decongestant is applied initially. The nasal valves are carefully examined without the use of a nasal speculum at first so as not to distort the natural anatomy. A speculum is then used to better evaluate the internal nasal valves. Still without decongestant, the patient is asked to grade his or her airflow through each side of his nose on a scale from 0 to 10. A cerumen curette is inserted into one side of the nose to gently support and lateralize the external and internal nasal valves. The patient is asked to grade the resultant airflow again from 0 to 10 while gently occluding the contralateral nostril.
The location of support that gives maximal improvement is carefully recorded. The procedure is then repeated on the other side. After decongestant is applied, the entire evaluation is repeated again to weigh the effects of mucosal edema on obstruction. These maneuvers, when combined with a thorough examination, can accurately predict the area of maximal obstruction and can help guide the surgeon as to the best surgical treatment.
Finally, the nose is examined endoscopically to exclude contributing pathology from the middle meatus or nasopharynx.
Specific Deformities of the Nose after Rhinoplasty
Upper Third
A successful rhinoplasty often will direct visual emphasis to a patient’s eyes in addition to enhancing the patient’s nose. Nasal bones too widely spaced may give the impression of telecanthus. Asymmetric shadows and bony irregularities of the nose may divert attention from the eyes. The bony width of the bony sidewall of the nose should be approximately 75% of the distance of a normal alar base on frontal view (Fig. 1-1). Deviations of the nose can be more readily appreciated by drawing a straight line from the midpoint between the brows to the upper lip and central incisors, provided there are no gross facial skeletal asymmetries (Fig. 1-1).
Two widths relate to the upper third of the nose: the nasal width and the facial width. The nasal width is the width created by each nasal bone as it traverses from the midline horizontally, before it curves toward the face. The facial width is the width created by the nasal bone and the nasal process of the maxilla as it traverses down to meet the horizontal face of the maxilla (Fig. 1-2).
Persistently wide nasal bones after previous rhinoplasty have several anatomic causes. The original surgeon may have performed either incomplete osteotomies (green stick fractures) or neglected to perform osteotomies all together. In patients with extremely wide nasal bones preoperatively, an intermediate osteotomy may have proven useful for further narrowing.3 Placement of the lateral osteotomy too far medially is likely to lead to palpable bony step offs.
Some patients have a persistently wide dorsum despite adequate lateral osteotomies. This may be caused by wide horizontal portions of the nasal bones, widening the nasal width without affecting the facial width of the nose. Excision of medial aspects of the nasal bones may be required to adequately reduce the nasal width in these patients (Fig. 1-3).
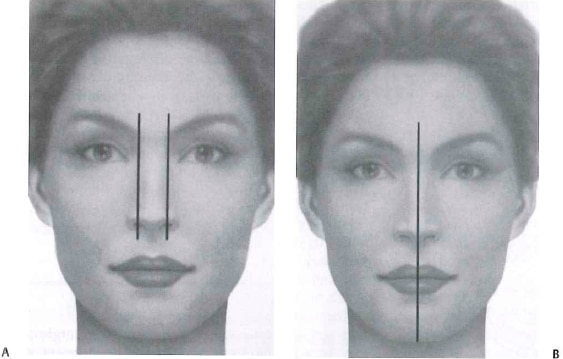
Figure 1 -1 (A) The ideal width of the upper one third of the nose is 75% of the distance of the alar base. (B) A midline drawn from the central glabella to central incisor may help better define any deviations of the nose (From Papel ID, Frodelj, Holt GR, Larrabee WF, et al. Facial Plastic and Reconstructive Surgery. 2nd ed. New York, NY: Thieme; 2002. Reprinted by permission.)
Overly narrowed nasal bones may result from osteotomies unnecessarily performed on an already narrow nose. A collapsed nasal bone can be the result of too aggressive a medialization of the nasal bone. Nasal bone instability also can be the result of overaggressive elevation or tearing of the overlying periosteum before osteotomies or violating the underlying mucoperichon-drium using wide osteotomes.
A “rocker deformity” occurs when the osteotomy takes place too far cephalically, onto the nasal process of the frontal bone. When the nasal bone is medialized, the superior segment narrows, but the caudal segment moves out laterally, causing visible deformity and persistent widening. As a general rule, osteotomies should either take place below the level of the medial canthus to avoid this deformity or course medially before arriving at the nasal process of the frontal bone.
Bony height discrepancy also may lead to persistent asymmetry. Lee, Kang, Choi, et al described performing an intermediate osteotomy in select cases to compensate for severely asymmetric bony vaults. A deviated radix, or root of the nose, may have gone undetected by the primary surgeon. A cross-root osteotomy is helpful in correcting this deformity.

Figure 1 -2 Width to the upper one third of the nose can be due to either the nasal or facial width. The nasal width is located dorsally along the bridge of the nose (red line on skull). The facial width is located along the nasal maxillary junction (green line on skull). Failure to appreciate these difference can lead to palpable step-off deformities and persistently wide nasal bones.
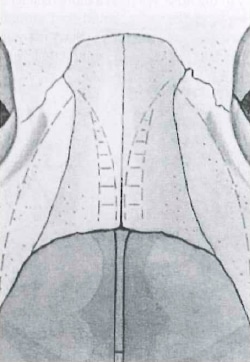
Figure 1-3 In extremely wide nasal bones, a wedge of bone may need to be removed to provide adeguate narrowing to the nasal pyramid.
Minor adjustments of the radix height can change the overall character of the nose. A high radix will impart a Romanesque quality to the nose, whereas a more balanced radix can impart elegance. The radix should start around the level of the supratarsal crease or upper ciliary margin. The radix height is usually analyzed in conjunction with the forehead shape and tip projection or dorsal height. The forehead orientation will affect the height of the radix. A flat forehead is less accommodating to a high radix than is a sloping forehead. The nasofrontal angle serves as a rough guide. The radix height relates to the angle formed between the frontal and nasal bones. Ideally, this angle should be between 115 and 130 degrees. Byrd and Hobar compared radix height with tip projection and dorsal height. They recommended using the plane of the cornea surface as a preferred reference point for radix projection. Radix projection, measured from the junction of the nasal bones with the orbit, is one third (0.33) the ideal nasal length. The radix projects 0.28 times the ideal nasal length from this surface (range: 9-14 mm) (Fig. 1-4) Likewise, McKinney felt the radix should be part of the balanced nose and defined this with the ideal ratio of 2:1:1:0.75 for length, projection, height, and radix, respectively7 (Fig. 1-5).
The anatomic cause of a raised radix may be a hump that was inadequately lowered. Conversely, the surgeon may have placed a radix graft larger than aesthetically desirable. A low radix may be the result of too aggressive removal of a nasal hump or a smaller than ideal radix graft.
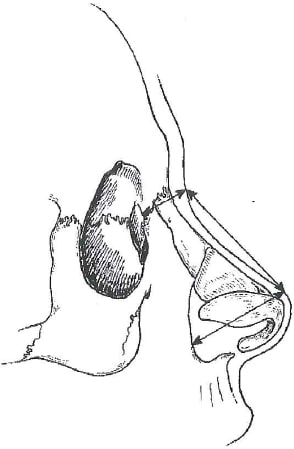
Figure 1 -4 Byrd and Hobar related radix height to ideal nasal proportions. The ideal nasal length is 0.67 the distance of the mid face height, and the radix height should be 0.28 of the nasal length (From Byrd HS, Hobar PC. Rhinoplasty: a practical guide for surgical planning. Plast Reconstr Surg 1993;91:642-656. Reprinted by permission.)
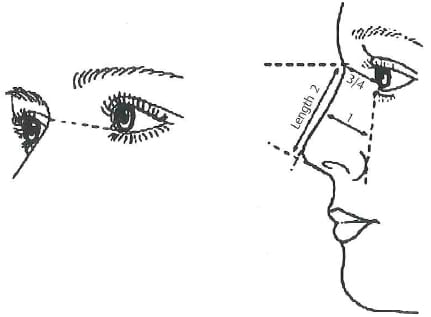
Figure 1 -5 McKinney and Sweis’s method of determining radix height is to compare it with either the rhinion or the projection. They state that in the ideal nose, the distance of the rhinion or projection is the same. The radix height is determined by drawing a line from the medial canthus to the nasal starting point. This distance should be three quarters the distance of either the nasal tip projection or the rhinion distance. This method relies on other variables of the nose being ideal, which is often not the case with either projection or the distance at the rhinion (From McKinney P, Sweis I. A clinical definition of an ideal nasal radix. Plast Reconstr Surg 2002;109:1419-1420. Reprinted by permission.)
Junction of Upper and Middle Third Nasal Bones and Upper Lateral Cartilages
One of the most common areas of patient dissatisfaction is the lack of smooth contour at the junction between the middle and upper one third of the nose. Diligent analysis compares the frontal and oblique views. The oblique view is essential in determining whether a persistent nasal hump is a midline or a lateral wall defect. The right oblique view provides information about the left nose and vice versa (Fig. 1-6).
There are several causes of either a visible or palpable deformity at this critical junction. A persistent “hump” may result from rasping the bone low, with the subsequent remaining high cartilage resistant to rasping. After removal of a dorsal hump, excessive upper lateral cartilage may be persistent and eventually cause disruption of both the functional and aesthetic outcome of the patient. Similarly, a spreader graft that has not been tucked under the nasal bone or secured adequately may manifest with a palpable edge. Inherent difficulties in correcting this area are compounded by the thin skin at the rhinion that is less forgiving in concealing nasal asymmetries.
An open roof deformity exists after bony hump removal without proper medialization of the nasal bones. Patients may present with depressed skin stuck down to intranasal mucosa and a persistently wide nose. An additional cause of open roof deformity is overzealous nasal packing, which can splint the nasal bones in a lateralized position. In patients with bony humps and low-lying nasal bones, a dorsal onlay cartilage graft may be necessary to conceal an open roof deformity.

Figure 1 -6 The oblique view serves to confirm the other views in rhinoplasty and places emphasis on the irregularities on the contralateral side. In this right-sided view of the patient, the dorsal hump’s convexity is more easily noticed on the left side of the nose. (Courtesy of M. Constantinides.)
Middle Third
The middle third of the nose provides the transition between the upper and lower thirds of the nose and should seamlessly blend with the rest of the nose. The ideal width on frontal view is variable but should be approximately 75% of the width of the ideal alar base. The height of the middle third of the nose should again be harmonious with the upper third and lower third. The height of the nose can be determined by drawing a line from the nasal starting point and to the anticipated tip position. The nose should lie at or slightly posterior to this line (Fig. 1-7). Any irregularities of the middle one third not only compromise aesthetic results but also may signal significant functional deficiencies.
Middle vault collapse has several anatomic etiologies. This deformity is often caused by aggressive dorsal resection without resuspension of the ULCs. This occurs when the ULCs and their mucosal attachments are severed from the dorsal septum and its mucosa resulting in inferomedial collapse. Patients with short nasal bones and long ULCs may be more susceptible to this phenomena.
Detached ULCs and a sharp dorsal septal edge, unilateral ULC collapse, and a deviated dorsal septum with ULC collapse or elevation are other scenarios that can lead to middle vault asymmetries. Overaggressive or imprecise rasping may lead to disarticulation of the ULC.
Saddle deformities can be caused be a variety of factors. When associated with a previous surgery, these deformities can be secondary to either an overaggressive dorsal reduction or, more commonly, a collapse of septal support after an aggressive septoplasty that failed to leave a sufficient L-shaped strut. Occasionally, an attempt to perform a caudal septoplasty for a severe caudal septal deflection may cause a small supratip saddle deformity. Postoperative etiologies include septal hematomas leading to abscess formation and bilaterally symmetrically torn septal flaps with chondrocyte death. Nonsurgical etiologies include cocaine abuse, granulomatous disease, syphilis, and neoplasms.
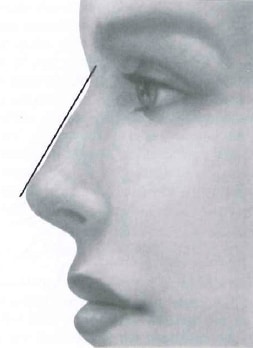
Figure 1-7 The dorsal height of the nose can be estimated by drawing a line from the nasal starting point to the ideal projection of the nose. The dorsum should lie at or slightly below this line.
Lower Third
The nasal tip represents the most complex anatomic nasal structure. Consequently, its analysis is equally challenging. The lower lateral cartilages are multifaceted, three-dimensional shapes that may have been altered by rhinoplasty to even more variant anatomy. The interaction between the lower lateral cartilages, the soft tissue envelope, and the septum are responsible for the overall shape and position of the nasal tip.
The projection of the nose can be measured in many ways. The Goode method involves comparing the distance from the alar facial groove to the tip to the nasal length and defines the ideal ratio as 0.55 to 0.6. (Fig. 1-8). Postoperative projection problems include the underpro-jected tip and the overprojected tip.
The underprojected nose in revision rhinoplasty often displays poor tip definition in thick-skinned or scarred patients and may be led by the anterior septal angle (tension nose). Underprojection occurs when one of the major tip supporting mechanisms is disrupted without proper stabilization. An example would be an endonasal delivery approach without subsequent support of the nasal tip. This technique violates a major tip support mechanism, the scroll, and may lead to deprojection of the nose. This may not be due to poor preoperative planning by the primary surgeon. At times, the dorsal height may have been adequately calculated in relation to the desired nasal tip height, only to have the nasal tip drop during postoperative healing. Reduction of the anterior septal angle, in this case, will only worsen the problem. Conversely, the postoperative overprojected nose often represents the primary surgeon’s failure to adequately deproject the nose intraoperatively.
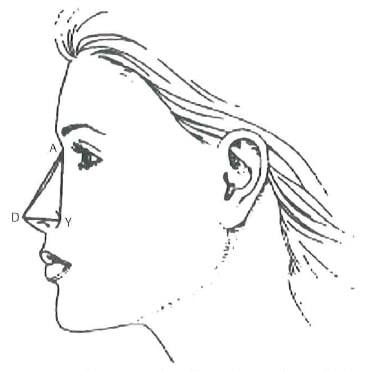
Figure 1 -8 The Coode method of measuring nasal projection draws a line from the nasal starting point to the nasal tip. The projection (DY) is compared with the nasal length (DA) and is ideally 0.55.
The amount of supratip break that is desirable depends on both surgeon and patient preferences. In a review of 882 cosmetic rhinoplasties (with a 7.1% revision rate), Stucker identified their primary deformity to be the pollybeak supratip deformity.” A pollybeak occurs when the supratip is the leading subunit of the nose. A high supratip area, in relation to the nasal tip, can have two etiologies. The most common is a high anterior septal angle. A careful examination with palpation is sufficient to make the diagnosis. Excessive soft tissue scar formation can be a second cause, commonly referred to as a “soft tissue pollybeak.” This occurs when an overzealous reduction in a thick-skinned individual creates a dead space that fills with soft tissue.
The transition between the nasal tip and the nasal ala should be smooth and without significant demarcations as seen from the frontal view. The ideal base view demonstrates a nasal tip with a triangular shape. Alar pinching presents with a narrow nasal tip and a steep drop off between the nasal ala and tip. This deformity can be caused by overaggressive resection of the lateral crura in an attempt to narrow the nasal tip. Alternatively, very tight dome-binding sutures can lead to pinching by making the nasal tip too narrow and breaking the normal smooth transition between the lateral crus and the dome. The ideal dome-binding suture leaves a flat contour to the lateral crus lateral to the suture. If the suture creates a concavity, tip knuckles and indentations can result during the postoperative recovery (Fig. 1-9). Finally, vertical dome division, the Goldman tip variant, when poorly executed can lead to a tent-pole deformity in which there are dramatic differences between tip and alar positions.
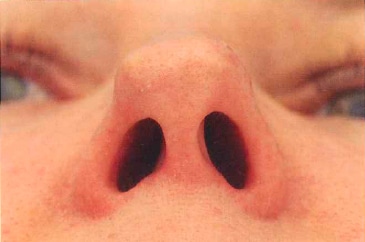
Figure 1 -9 Patient exhibiting classic bossa-like formation of nasal tip secondary to previous rhinoplasty performed by outside surgeon. Also note the knuckle of the right dome. (Courtesy of M. Constantinides.)
In patients with excessive columellar show, it is important to differentiate between alar retraction and a hanging columella. The ideal amount of columellar show is 2 to 4 mm. The amount of columellar show can be measured by the method presented by Rohrich and Gunter. To establish the exact etiology, a line is drawn bisecting the nostril on the lateral view (Fig. 1-10). The distance from the alar rim to this line (A to B) should be equal to the distance from the caudal edge of the columella to the line (C to B). Excess in the superior area (A to B) is caused by alar retraction, whereas excess in the inferior area (C to B) is caused by columellar excess. Columellar excess can be caused by either a weakened medial crural complex after rhinoplasty or by an overly long caudal septum, prominent nasal spine, or both. Palpation of the medial crura and the caudal septum will detect the deformity and allow for its correction.
The nasal ala can become retracted from aggressive lateral crural resection during rhinoplasty. The resection of vestibular mucosa during cephalic resection also may contribute to the retraction. Postsurgical scarring elevates the alar rim when there is a deficiency of the cartilage. Patients with cephalically positioned lower lateral cartilages are especially at risk for retraction. Because of an already-deficient lateral lower lateral crus, excision of cartilage may lead to notching of the nostril.
Deviation of the columella can be caused by several factors. If the caudal septum is deviated, often the columella will follow it. If a footplate is prominent and asymmetric, it may give the appearance of a columellar deviation. In some patients with weak medial and intermediate crura of the lower lateral cartilages, the columella may deviate because of poor underlying structural support.
The external nasal valve consists of the alar rim and the fibrofatty tissue in the nasal ala. Collapse of this structure can occur naturally in patients with inherent weakness. However, aggressive resection of the lateral crura can lead to a weakened external valve unable to resist the negative pressure of inspiration.
Nasal tip asymmetries can be assessed from all views, but the base view often provides useful information. The nasal tip should be triangular in shape when viewed from the base with a ratio of columella to tip lobule of approximately 2:1. The base view provides perspective on alar pinching and discrepancy in tip height. The width of the nasal lobule should be 75% of the entire nasal base. The causes of tip asymmetry are varied. Unequal excision, suturing, or shifting of graft are all possibilities. Asymmetries of the tip occurring later can be due to unequal scar forces or thin skin contracture unveiling a once hidden asymmetry.
A tip bossa, or broad convexity of alar cartilage, can occur spontaneously or in a cartilage remnant adjacent to a previously resected portion of cartilage. Kamer and associates reported this deformity as the most common nasal-tip deformity in patients undergoing revision surgery. However, this study was a retrospective examination of endonasal rhinoplasty. Domal bossae may occur when the lower lateral cartilages are aggressively resected, leaving a sharp edge in which the S-STE contracts around the domal area. This also may occur when the domes are sharply divided.
Knuckles develop from an overly weak segment of cartilage that bends upward during the healing process. A knuckle also can be the result of an overtightened dome-binding suture.
Tip grafts may become visible with time. Often the forces of scar contracture will reveal previously hidden grafts placed in the tip lobule or columella. Poorly secured grafts can easily become displaced during scar contracture. Tip grafts should be avoided when possible in thin-skinned patients. The edges should be thinned and trimmed so that no edge is seen nor felt. Camouflage with perichondrium, crushed cartilage, temporalis fascia, or acellular dermis may be necessary to prevent tip graft visibility.
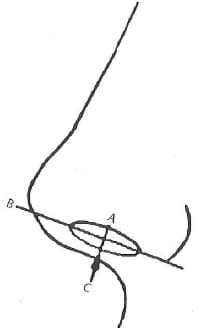
Figure 1-10 Gunter and Rohrich defined the normal alar-columel-lar relationship by drawing a line (B) from the anterior most point of the nostril to the posterior point. The distance to either the columella or alar rim should be 1 to 2 mm. See text. (From Gunter JP, Rohrich RJ, and Friedman RM. Classification and correction of alar-columellar discrepancies in rhinoplasty. Plast Reconstr Surg 1996;97:643. Reprinted by permission.)
Junction of Nose and Lip
The nasolabial angle also can be measured in several different ways. One method is to measure the angle created by a line from the anterior nostril to the posterior nostril, along the long axis of the nasal rim, and a vertical line perpendicular to the Frankfort horizontal line (Fig. 1-11). Another method is to measure a line from the subnasale to the superior vermilion and by a tangent of the columella from the subnasale. The aesthetic ideal for the nasolabial angle is defined by a range of 90 to 105 degrees in men and 95 to 115 degrees in women.16 Some authors stress the difference between columellar labial angle and nasolabial angle to distinguish a hanging columella from a ptotic tip. In a patient with a hanging columella, the angle between the tip in relation to a vertical tangential plane of the face may be obtuse. In a patient with a ptotic tip, this angle is acute (Fig. 1-8). The superiorly rotated nose can be a result of excess anterior septal angle resection or poor placement of a tip graft. The inferiorly rotated nose is most often the result of deficient medial crural support. Inattention to loss of tip support after reduction rhinoplasty in a tension nose is a less common cause.
A lack of double break can be a tell-tale sign of a shield graft. Camouflaging the lower border of the tip graft with crushed cartilage or scoring the cartilage to allow a small amount of curvature in the inferior portion of the graft will help in preventing this.
A prominent posterior septal angle can be difficult to correct. Patients with such a deformity also may have the illusion of a shorter, tense upper lip. It can result from residual posterior septum or nasal spine. Conversely, some patients will have an overreduced posterior septal angle that may result in a retracted, long upper lip. Resection of the depressor septi nasi muscle can improve the inferior pull on the tip, but can lead to a smile that shows less of the upper teeth if overdone.
The width of the alar base can be assessed by frontal view. It should be approximately the same width as the intercanthal distance. However, variability exists between ethnicity. Powell and Humphreys defined ideal alar width as the distance between the alar facial grooves equaling 70% of the length of the nose.20 Guyron recommended interpretation of the alar base in context with the surrounding structures and ideally is located 1 mm outside the intercanthal distance (Fig. 1-12).21
The persistently wide alar base is a surgical error of omission (failure to adequately resect tissues). This may occur because of change in nasal dynamics not anticipated by the surgeon, such as deprojection of the nose causing flaring of the nostrils or placement of alar rim grafts pushing nostrils laterally.22 Conversely, the overly narrow alar base, an error of commission (aggressive resection of tissues! is much more difficult to correct.
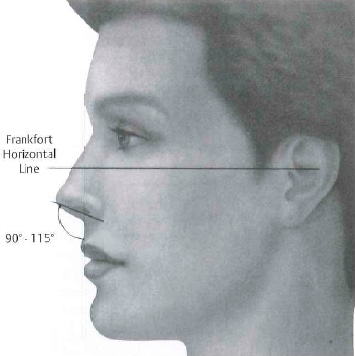
Figure 1-11 The nasolabial angle can be assessed in two ways. A line through the axis of the nostril compared with a vertical tangent to the Frankfort horizontal provides accurate location of tip angle. An alternate technique that creates an angle from the line created by the upper vermillion border to the subnasale to the most prominent point of the columella is susceptible to misinterpretation with hanging columellas, prominent nasal spines, and other nasal deformities. (From Papel ID, Frodel J, Holt CR, Larrabee WF, et al. Facial Plastic and Reconstructive Surgery. 2nd ed. New York, NY: Thieme, 2002. Reprinted by permission.)
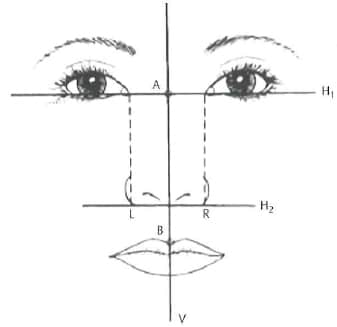
Figure 1-12 Alar base diagram. The conventional technique for analyzing alar base width is to draw two parallel lines from the medial canthus (assuming normal intercanthal distance). Guyron proposed the base should be 1 mm wider (From Guyuron, B. Dynamics in rhinoplasty. Aesthetic Plast Surg 2002;26(Suppl 1 ):10. Reprinted by permission.)
Conclusion
The analysis of revision rhinoplasty and its underlying structural cause is an insight into the complications of rhinoplasty. Aggressive reductive techniques without structural support will lead to long-term unpredictable outcomes. Contextually deviant and poorly executed technique will often impart the stigmata of an unsuccessful rhinoplasty as well.
Revision rhinoplasty requires proper planning and understanding of the aberrant anatomy. An appreciation of individualized facial proportion and symmetry with recognition of the structural deficiencies or excess will allow for more favorable rhinoplasty outcomes.

