Aesthetic and Functional Correction of the Nasal Base
Jack D. Sedwick, MD; Andres Bustillo, MD; Byron J. Gajewski, PhD; Robert L. Simons, MD
Objectives: To describe our technique in the treatment of significant caudal septal deviation; to evaluate the effectiveness of our technique of caudal septoplasty in the treatment of caudal septal deviations.
Design: Retrospective review of cases taken from a database of more than 2000 patients who underwent rhinoplasty performed by 1 surgeon in a private facial plastic surgery practice.
Results: Medical charts were reviewed to determine the rate of preoperative nasal obstruction in 59 (95%) of 62 patients as well as nasal obstruction postoperatively 11 (17%) of 62 (P<.001). Photographs were reviewed to determine the severity of caudal deviation and the postoperative result. By photographic evaluation, we found that all but 3 patients had significant improvement in their postoperative appearance. Twenty-six patients had no evidence of residual asymmetry. The rate of revision was 5
(8%) of 62 patients.
Conclusions: The caudal septoplasty technique is effective, relatively easy to perform, and shows long-term reliability in correcting caudal septal deviation. In properly selected patients, the technique is effective in improving cosmesis and nasal airflow.
Arch Facial Plast Surg. 2005;7:158-162
THE CORRECTION OF CAUDAL septal deviations can be a challenging problem. Often, these defects cause both an aesthetic distortion of the nasal base and nasal obstruction. The fact that so many techniques have been described and tested to correct caudal septal deflections speaks to the difficulty of correcting this problem. If it were easily corrected, 1 technique would probably be used more universally.
The present study describes a technique used by the senior author (R.L.S) for more than 20 years and evaluates its effectiveness in managing caudal septal deviations. We believe that effective treatment of caudal septal deviations significantly improves outcomes in rhinoplasty. The deviated caudal septum changes lobular and columellar relationships and has a significant effect on tip position and symmetry. In some cases, treatment of the caudal septum can significantly improve a twisted nose. In selected cases, this may be the most important element in treating a twisted nose. The present review concentrates on the effect of caudal septoplasty on the appearance of the base of the nose and on breathing.
METHODS
PATIENT ENROLLMENT
Patients were selected from a rhinoplasty database in which information regarding patient demographic characteristics, preoperative analysis, operative techniques, and complications were recorded. All patients undergoing rhinoplasty by the senior author over the last several years were entered into the database without intentional bias. A total of 2043 cases were available for review and inclusion in this study. All operations were performed in either a community hospital or an officebased surgery suite.
All patients were entered into the rhinoplasty database in a randomized fashion, without any consideration given to use of these data in the present study or any other study. The original database of 2043 patients was searched for patients with caudal septal deviation noted and recorded in the preoperative evaluation of patient photographs. This search was then matched with patients who had a caudal septoplasty for treatment of caudal septal deviation. In virtually all cases, the caudal septoplasty was performed in conjunction with an endonasal cosmetic rhinoplasty.
These search parameters yielded 147 patients (8%) who had a caudal septal deviation treated with a caudal septoplasty. All of these medical charts were reviewed. Complete charts were included in this study, along with complete preoperative and postoperative photographic information, documentation of subjective breathing status before and after surgery, and at least 6 months of postoperative follow-up records. Patients treated with turbinate reduction, internal or external nasal valve repair, or any technique designed to improve breathing other than caudal septoplasty were excluded from the review. A total of 62 patients met these criteria and were included in the study.
These 62 charts were reviewed to determine the subjective rates of nasal obstruction before and after treatment in a retrospective manner. Two independent observers evaluated the severity of preoperative caudal septal deviation and the effect of surgical intervention. The rate of revision surgery in this patient group and the length of follow-up were recorded as well.
SURGICAL TECHNIQUE
Caudal septoplasty was performed in conjunction with endonasal rhinoplasty in each case. Patients who underwent turbinate reduction or internal or external valve repair were excluded from this study. The septum was accessed via a complete transfixion incision. In each case, this incision was ultimately used in conjunction with an intercartilaginous incision and a marginal incision to perform the rhinoplasty. Bilateral mucoperichondrial flaps were elevated via a complete transfixion incision in each case. Bilateral flap elevation allows the surgeon complete bilateral access to the caudal septum from the anterior septal angle to the nasal spine.
After the septum was accessed via the complete transfixion incision, deviated cartilage was excised using standard septoplasty technique leaving at least a 1-cm caudal and dorsal strut to preserve the structural function of the caudal and dorsal septum. Next, the caudal septum was exposed to the nasal spine via the complete transfixion incision using bilateral mucoperichondrial flaps. With this access, the caudal septum was positioned over the nasal spine in the midline and straightened.
Often the length of caudal septal strut contributes to the deviation. When this occurred, we shortened the most posterior aspect of the caudal strut so that it could be placed without deviation over the nasal spine in the midline. In cases where the caudal septum was malpositioned without additional length contributing to the deviation, we repositioned the septum to one side or the other of the nasal spine. Through the access provided by the complete transfixion incision, the septum can be repositioned to the midline with bilateral visual verification of its position.
Once the caudal septum was successfully repositioned in the midline, it was secured in that position so that the newly straightened caudal septum remained in its proper position. The newly positioned caudal strut was then secured to the columella using 4-0 chromic gut suture on a straight needle to hold it in the midline position while healing took place. Multiple septal columella sutures can be placed, although 1 or 2 sutures are usually sufficient. The caudal septum was not secured to the nasal spine. Closure of the posterior portion of the transfixion incision was meticulously performed to provide added strength and support prior to continuing with the rhinoplasty. We believe that placement of Telfa packs (Tyco Health Care, Mansfield, Mass) at the conclusion of the procedure helps to support the incisions, including the complete transfixion incision and the intercartilaginous incision. Telfa sponges are left in place for 2 days in all cases. Standard casting is performed postoperatively.
RESULTS
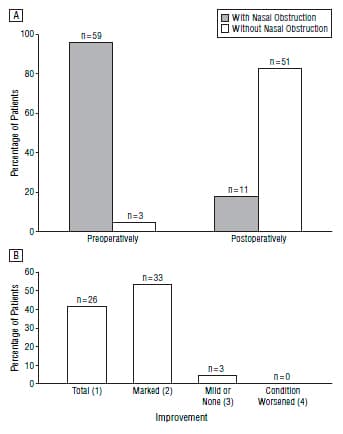
Figure 1. Patient self-reports of nasal obstruction (A) and physician photographic evaluations of aesthetic improvement (B). A, Improvement in nasal obstruction was significant (P<.01, McNemar test). B, The aesthetic surgical results were evaluated on a 4-point scale: 1, little or no photographic evidence of residual caudal septal deviation (total improvement); 2, marked improvement; 3, only mild or no improvement; and 4, condition made worse. In none of the present cases was the condition made worse. Improvement was statistically significant (P<.001).
The patients’ charts were reviewed to evaluate the rate of subjective nasal obstruction preoperatively. Figure 1 A summarizes these results. The initial result indicated that 59 (95%) of the 62 patients complained of nasal obstruction during their initial consultation. The degree of nasal obstruction could not be recorded owing to the retrospective manner in which the charts were reviewed. The charts were reviewed for postoperative complaints of nasal obstruction as well. Charts in which patients’ subjective opinions regarding the status of their airway at their last follow-up appointment were not clearly documented were excluded from the study. Fifty-one (82%) of 62 patients reported no postoperative nasal airway obstruction. All of the patients with residual airway obstruction reported improvement in their breathing status. The difference between the rates of preoperative and postoperative nasal obstruction was statistically significant(P<.01).
The results of the surgery with respect to improvement of the caudal deviation were evaluated using the base photographic view. In all cases, the most recent photographs were used to evaluate the postoperative result. All patients without photographic evaluation at least 6 months after surgery were excluded from the study.

Figure 2. Preoperative (A) and postoperative (B) base views of a patient with a caudal septal deviation that was judged by both evaluators to be completely corrected (score, 1) by caudal septoplasty.

Figure 3. Preoperative (A) and postoperative (B) lateral views of the patient pictured in Figure 1.
A 4-point grading system was used to evaluate results. A score of 1 indicated that the patient had little or no photographic evidence of residual caudal septal deviation; 2, the caudal septal deviation showed marked improvement but was still detectable by careful observation; 3, the caudal deviation was only mildly improved or not improved from the preoperative assessment; and 4, the caudal deviation was worse after surgical intervention. Two independent observers reviewed the photographs, and the scores of these observations were averaged. The average result for all patients was 1.6. These results are summarized graphically in Figure 1B and were statistically significant (P<.01). No conditions were worsened by the surgery. Twentysix patients had complete improvement (score, 1), and 33 showed marked improvement (score, 2) in their most recent photographs.
Figure 2 and Figure 3 show a female patient with a severe caudal septal deviation, before and after caudal septoplasty. Although the photographs were scored from the caudal view, the lateral views are included for reference. This patient’s result was scored as 1 by both observers. Figure 4 and Figure 5 show a male patient with a severe caudal septal deviation. The postoperative result in this case was scored a 1 by one observer and a 2 by the second observer.
The rate of revision rhinoplasty as well as the duration of follow-up were recorded in this group of patients. Five (8%) of 62 patients underwent revision surgery. This rate of revision is similar to that of all patients undergoing rhinoplasty with the senior author (3%-8%). The reasons for revision surgery varied in this small group of patients: synechine in 2 patients, a residual twisted nose in 1 patient, an overprotected dorsum in 1 patient, and implant reaction in the final patient. In all cases, revisions were performed for reasons other than dissatisfaction with the result of the caudal septum. Most of these patients had deformities in addition to caudal septal deviation, and all underwent procedures in addition to caudal septoplasty for treatment of these deformities.


Figure 4. Preoperative (A) and postoperative (B) base views of a patient with a caudal septal deviation that was rated postoperatively to be completely corrected(score, 1) by one observer and markedly improved (score, 2) by the seond observer.
Figure 5. Preoperative (A) and postoperative (B) lateral views of the patient pictured in Figure 4.
Patient follow-up was recorded as well. All patients with less than 6 months of clinical and photographic follow-up were excluded from this study. Many patients traveled some distance for surgery and were unable to return for complete follow-up owing to distance and cost. The average duration of follow-up was 21.5 months(range, 6-180 months).
COMMENT
In his description of the traditional septoplasty, Freer stressed the importance of an L-shaped caudal and dorsal strip of cartilage to avoid external nasal deformities. This technique does not address caudal septal deflections. Resection of the caudal margin of the septum has the potential to disrupt the aesthetics of the columella as well as disrupting tip support. Since Freer’s early work, several authors have described procedures used to correct caudal septal deflections.
Metzenbaum was one of the first to describe a procedure for the correction of the caudal septum. He recognized the importance of its preservation for nasal support. His technique called for the mobilization of the caudal septum to the midline in a “swinging door” fashion. Various methods of formal suturing of the posterior inferior margin of the cartilage to the nasal spine have been described.
Ellis described his use of Mustarde-type nonabsorbable sutures on the concave side to correct the deviation. Others have described techniques of scoring the concave side of the caudal deviation. These techniques weaken the cartilage and are associated with a high failure rate in the long term.
Anderson described the ethmoid bone sandwich graft, in which small bone grafts are placed on each side of the caudal septum to maintain it in the midline. In his limited study, 8 of 10 patients maintained satisfactory correction of their caudal defect.
Recently, Pastorek described his “modified swinging door” technique in which the caudal septum is flipped over the nasal spine, which acts as a doorstop holding the septum in the midline. A suture is then used to secure the septum to the spine.
Kridel describes the “tongue in groove” technique for the management of caudal deviations. The procedure involves placement of the caudal septum into the groove between the medial crura to hold it in place. This procedure would tend to shorten the nose. In a recent study with 108 patients undergoing his technique, all claimed to have satisfactory results, and none required revision surgery.
For severe caudal septal deflections, Toriumi has advocated the removal of the entire L-shaped strut and replacement with septal cartilage. Although this is a potentially effective procedure, it requires a large amount of straight cartilage as well as a much more aggressive dissection via an external approach. The potential for loss of nasal support due to graft loss may be greater than with other less aggressive techniques.
Over the past 20 years, our technique has been extremely beneficial in the management of caudal septal deviation. This technique calls for cartilage preservation in the area of the caudal septum. It avoids loss of tip support and the creation of a retracted columella. Although the resection of the caudal septum may be beneficial to correct a hanging columella or a long nose, it cannot be used in every nose. The scoring or shaving of the columella may reduce the strength of this vital area of loadbearing cartilage and lead to loss of tip support or unpredictable scarring
The technique described is effective, is relatively easy to perform, and shows long-term reliability in correcting caudal septal deviation. In properly selected patients, the technique is effective in improving both cosmesis and nasal airflow. We did not encounter complications involving scarring or loss of tip support. The nasal tip remains natural in appearance, and the results are functionally and aesthetically pleasant.
This review is a large series with careful statistical analysis that evaluates the management of the caudal septum. Using this procedure in 62 patients with a minimum of a 6-month follow-up, we effected improvement in postoperative appearance for most patients. Most patients also had normal nasal airflow postoperatively. Both aesthetic improvement and improvement in nasal airflow were statistically significant. The rate of revision surgery in this group of patients was not significantly different than that of patients undergoing standard rhinoplasty.
REFERENCES
1. Freer OT. The correction of the deflections of the nasal septum with a minimum of traumatism. JAMA. 1902;38:636.
2. Metzenbaum M. Dislocation of the lower end of the nasal septum cartilage. Arch Otolaryngol. 1936;24:78.
3. Ellis MS. Suture technique for caudal septal deviations. Laryngoscope. 1980;90: 1510-1512.
4. Wright WK. Principles of nasal septum reconstruction. Trans Am Acad Ophthalmol Otolaryngol. 1969;73:252-255.
5. Anderson JR. Ethmoid bone sandwich grafting for caudal septal defects. Arch Otolaryngol Head Neck Surg. 1994;120:1121-1125.
6. Pastorek NJ. Treating the caudal septal deflection. Arch Facial Plast Surg. 2000;2: 217-220.
7. Kridel RW. The tongue-in-groove technique in septorhinoplasty. Arch Facial Plast Surg. 1999;1:246-256.
8. Toriumi DM. Subtotal reconstruction of the nasal septum: a preliminary report. Laryngoscope. 1994;104:906-913.

